Certified Error Rate Testing CERT audits. The auditor collects a small sample of claims to review for compliance.
 3 Things You Need To Know About Medicare Audits Medconverge
3 Things You Need To Know About Medicare Audits Medconverge
The due date is not the last date on which you can mail the records but rather is the date that the records must be at the auditors office.
When are medicare audits done. This section explains that the changes to OfficeOther Outpatient EM Services 99201-99215 which have been scheduled for implementation on January 1 2021 could immediately be implemented retroactive to March 31 2020 for telehealth EM services provided to Medicare. If a provider is selected to undergo a UPICZPICRACMAC or similar medicare audit it is either because it is already the subject of a fraud investigation or ZPIC is seeking to gather more information to determine whether such an investigation should be opened. MHK will host a webinar in September on this topic.
Audits and Appeals Overview. Congratulations on your recent Medicare audit results. Level Selection for OfficeOutpatient EM Visits When Furnished Via Medicare Telehealth of the CY 2020 PFS final rule 84 FR 62847 and 62848.
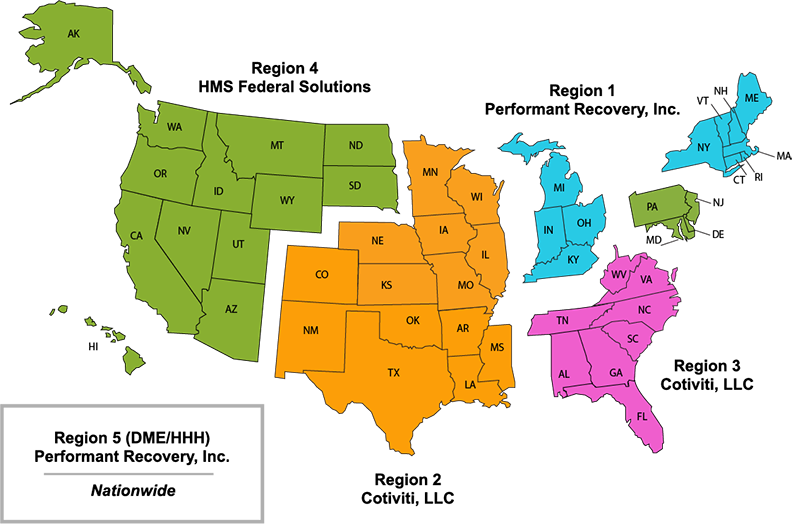
After successfully passing a three-month UPIC Medicare Unified Program Integrity Contractor audit your network then underwent a subsequent TPE Medicare Targeted Probe and Educate program audit. The purpose of this web page is to increase transparency related to the Medicare Advantage and Prescription Drug Plan program audits and other various types of audits to help drive the industry towards improvements in the delivery of health care services in the Medicare Advantage and Prescription Drug program. You will often find that the Medicare audit and the site visit will occur at the branch office that appears on the claim form that you submit to the CMS.
Be on the lookout for an invitation. According to the CMS website CERT audits are conducted annually using a statistically valid random sample of claims Auditors review the selected claims to determine whether they were paid properly under Medicare coverage coding and billing rules Probe audits. Medicare contractors are bound to follow all NCDs when they adjudicate or audit Medicare claims.
Oh and lower is better so heres to hoping the trend continues. Backlog effectively denies suppliers any remedies they may have had under the Medicare appellate process. Medicare audits are one of several things that can trigger a larger civil or criminal investigation by federal law enforcement.
The TPE audit scored 100 out of 100 possible points. For the 13 audits in 2019 that dropped to 077. Once the status has been determined ie services were or were not reasonable and necessary the claim will be processed.
As we learned the demonstration as proposed would allow Medicare recovery auditors to review claims after services are provided but before claims are paid to ensure that the provider complied with all Medicare payment rules. When receiving a notice of a Medicare audit time is of the essence. For the most partauditors are professional and do their best to conduct fair audits.
Contractors may develop local coverage determinations LCDs that do not conflict with NCDs. Preparing and Maintaining Supporting Documentation. Usually auditors con-clude that Medicare has made signiWcant over-paymentsand demand that the audited physician return the money.
She then determines the error rate of the sample. For example if 50 claims are reviewed and 10 are found to. If the visit is at a branch office make sure the right personnel are there.
The scheme only applies to audits commenced from 1 July 2019 in relation to services provided from 1 July 2019 onwards. The auditors review the selected claims and determine whether those claims were paid properly under Medicare coverage coding and billing rules. The majority of DRG coding errors are due to up-coding.
DRG audits are very straightforward reviews to ensure that the services provided match the diagnosis code billed. If you have been through an audit and are required to repay Medicare billings you should consider the income tax implications of any repayment of funds. Specifically CMS is suspending pre-payment medical reviews done by Medicare Administrative Contractors MACs under the Targeted Probe and Educate TPE program and most post-payment reviews conducted by MACs Supplemental Medical Review Contractors and Recovery Audit Contractors.
Medicare contractors with the responsibility to audit are given the same guidelines regarding the type of review and reasons to deny. Our legal team has decades of experience with the Medicare audit process and can help you as well. Therefore providers should recognize that a ZPIC Audit.
If a DRG code is found to be incorrect it is corrected by the auditor the payment is. Why are DRG audits so simple. The primary purpose of a Medicare Audit as opposed to a random inspective audit is to identify fraud.
Be sure to calendar the date that the records need to be in to the auditor and have the records there by that date. Extrapolation is the tsunami in Medicarecaid audits. If a visit is to.
This paragraph was located in the section titled W. There is never an outright denial of the claim. CERT Audits As per the Centers for Medicare and Medicaid Services CERT audits are conducted on an annual basis using a statistically valid random sample of claims.
Providers should retain ALL relevant supporting documentation in either paper or electronic format used in the completion of the Attestation Module responses for six years post-attestation. Prepayment review of claims always results in an initial determination and is assessed on the current claim.