Telehealth Coverage for the Oregon Health Plan and a bit about other payers Prioritized List of Health Services effective 3132020 Guideline Note A5 TELECONSULTATIONS AND ELECTRONICTELEPHONIC SERVICES Statement of Intent 6 TELEPHONIC SERVICES DURING AN OUTBREAK OR EPIDEMIC httpswwworegongovohaHPADSI. Our states have significant individual and collective experience with telehealth.
 New Oregon Telehealth Laws To Assist Providers With Covid 19 Pandemic Efforts Stoel Rives Health Law Insider Jdsupra
New Oregon Telehealth Laws To Assist Providers With Covid 19 Pandemic Efforts Stoel Rives Health Law Insider Jdsupra
See the rules for physicians to practice medicine across state lines in OAR 847-025.
Oregon medicaid telehealth. O Telehealth services shall be available for all conditions not just COVID-19 or suspected COVID-19 cases as medically and clinically appropriate. Operational and billing information for Oregon Health Plan Medicaid providers and coordinated care organizations. This guide acts as the single source for Oregon Medicaid provider guidance including telehealth related to provision of services under Medicaid during the COVID-19 emergency declaration.
Throughout this pandemic telehealth has provided Oregonians with essential access to health care services that otherwise might have been unavailable or required the risk of an in-person appointment said Gov. O Health plans shall allow both existing and new patients to access health care including behavioral health and substance use disorder services without risking spread or transmission of COVID-19. This document summarizes existing and new.
It has transformed how many people have accessed behavioral health services. The Oregon telehealth mandate Alaska group and individual medical plans issued or renewing 1012016 and after any Alaska ASO plans which adopt the Alaska telehealth mandate Medicare Advantage plans and Oregon Medicaid plans. Telehealth allows for Oregonians to get important care often from the comfort of their home.
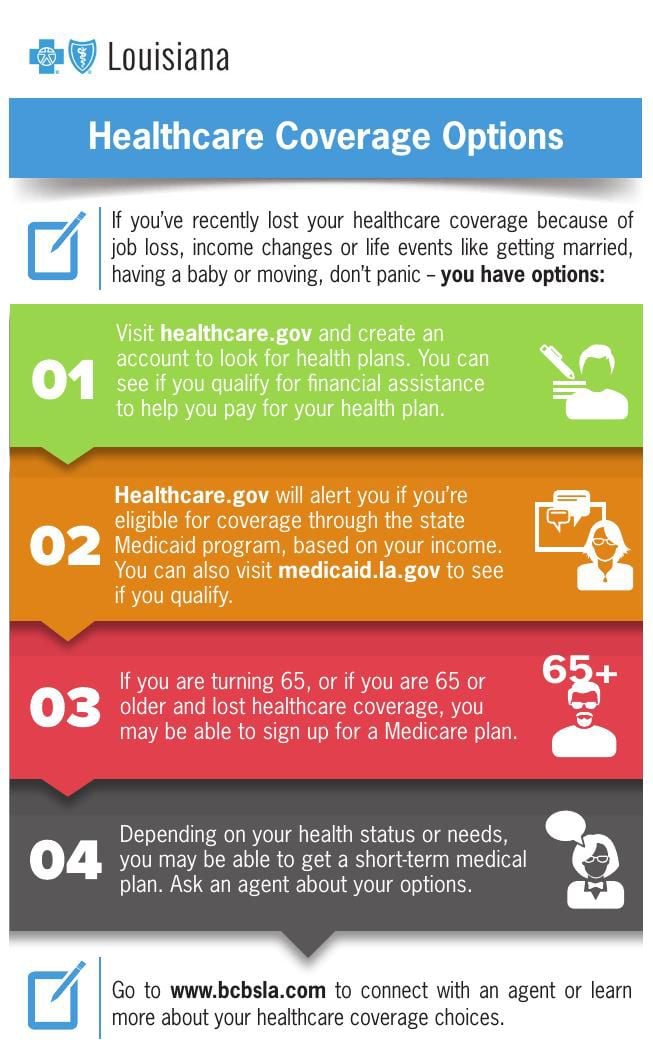
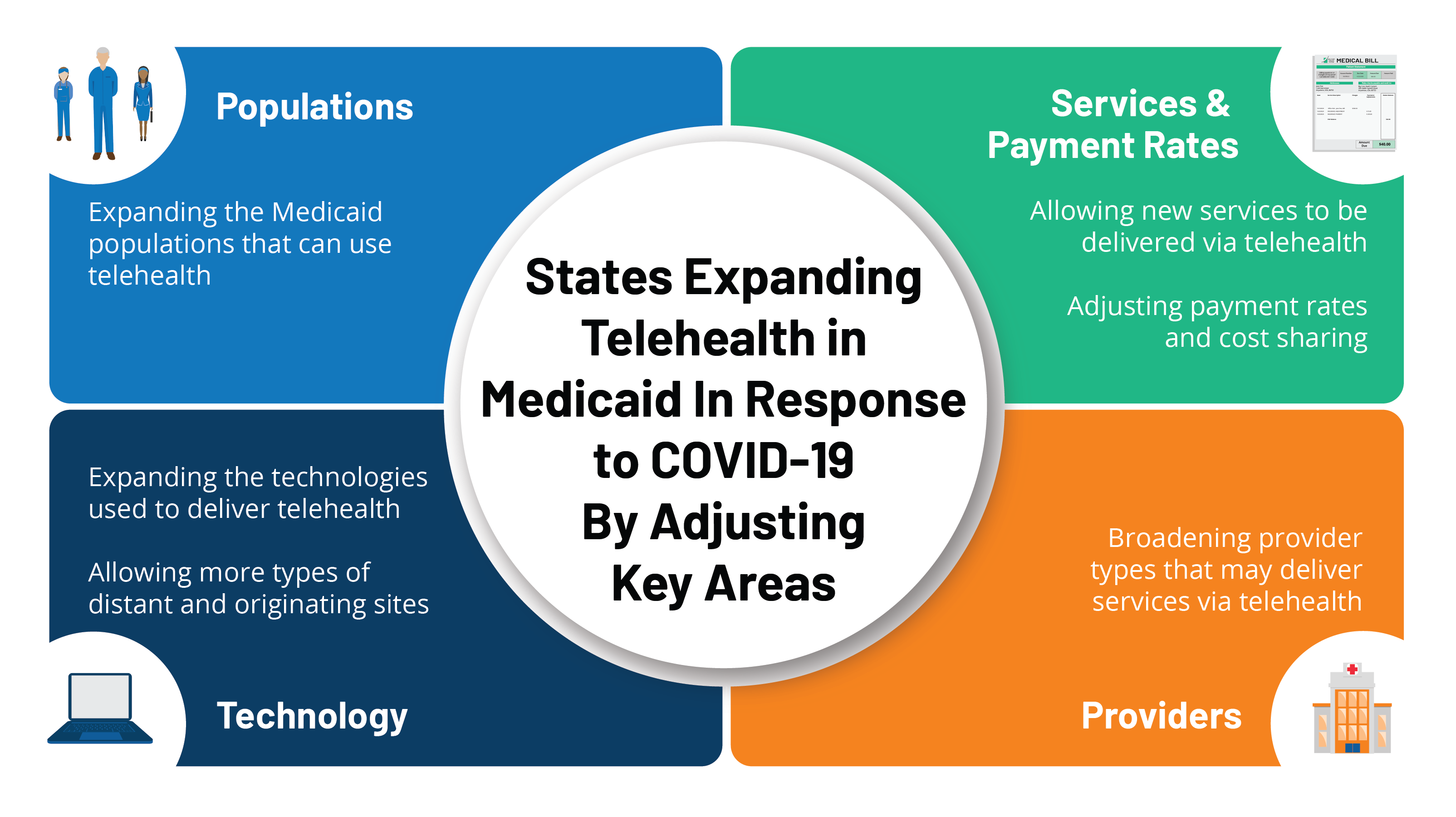
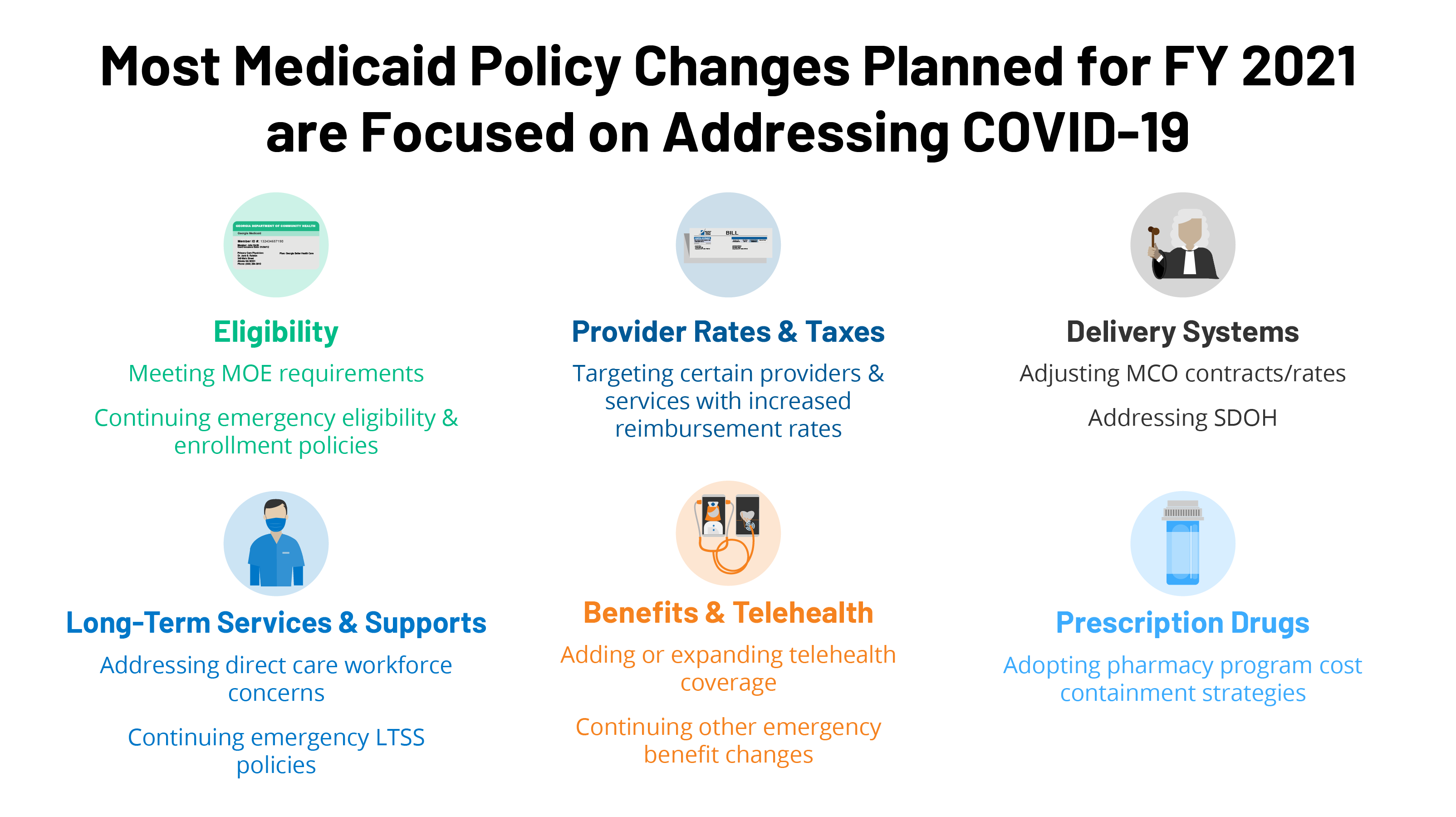
The federal Center for Medicare and Medicaid Services CMS has recently announced its intention to make permanent some of the telehealth flexibilities afforded during this pandemic. OHA is expanding coverage of telehealth and telephone services in light of the COVID-19 outbreak. Current guidance regarding covered services telemedicine eligibiliity prior authorization and billing.
The State of Oregon has reached an agreement with several health insurance companies to continue providing expanded telehealth options through at least June 30 2021. Oregon Democrats Lead on Ensuring Equity and Access to Telehealth Services SALEM The Oregon Senate passed House Bill 2508 a bill to ensure telehealth care reimbursement is aligned with other health care services. During the COVID -19 pandemic the Oregon Health Plan OHP is expanding coverage for the delivery of physical behavioral and oral.
The bill also makes certain that telehealth care is more broadly available during states of emergency. Resources for Oregon Health Plan providers and CCOs. Telemedicinetelehealth services Oregon Health Plan coverage of telephonetelemedicinetelehealth services Information for Oregon Health Plan physical and behavioral health providers Whats new.
This work will contextualize and catalog the telehealth services provided at Oregons Rural Health Clinics RHCs. It is vital for Oregonians to continue to use telehealth services to limit physical contact during this public health emergency said Oregon Insurance Commissioner and Department of Consumer and Business Services Director Andrew Stolfi. Please refer to the Oregon Medicaid COVID-19 Provider Guide for.
Prescribes requirements for reimbursement by Oregon Health Authority and coordinated care organizations of health. Evaluation and management services. Telemedicine visits are encouraged for all services that can reasonably approximate an in- person visit not just those relating to a COVID -19 diagnosis.
Medicaid Telemedicine and Telehealth Overview and Guidelines as of 3262020 OVERVIEW In light of the COVID-19 pandemic the Oregon Health Authority has expanded coverage of telehealth services. The following telehealth and telemedicine services are covered through OHSU Health Services. Telehealth is here to stay.
The Oregon Health Science University Telemedicine Network provides immediate patient access to pediatric neonatal stroke neurosurgery and other specialists throughout Oregon 247. The Oregon Office of Rural Health ORH is managing a new project in partnership with the Telehealth Alliance of Oregon TAO and the Northwest Regional Telehealth Resource Center NRTRC. OHA COVID-19 Telehealth Provider Webinar Medicaid The Oregon Health Authority OHA is providing this webinar to cover a variety of questions OHA has received about the Oregon Health PlansMedicaid coverage of telehealth services during.
TelehealthTelemedicine are terms used interchangeably. For Oregon a Telemedicine Active status license is for physicians who practice entirely outside of Oregon and render medical treatment to patients in Oregon via electronic means. House Bill 2508 was.