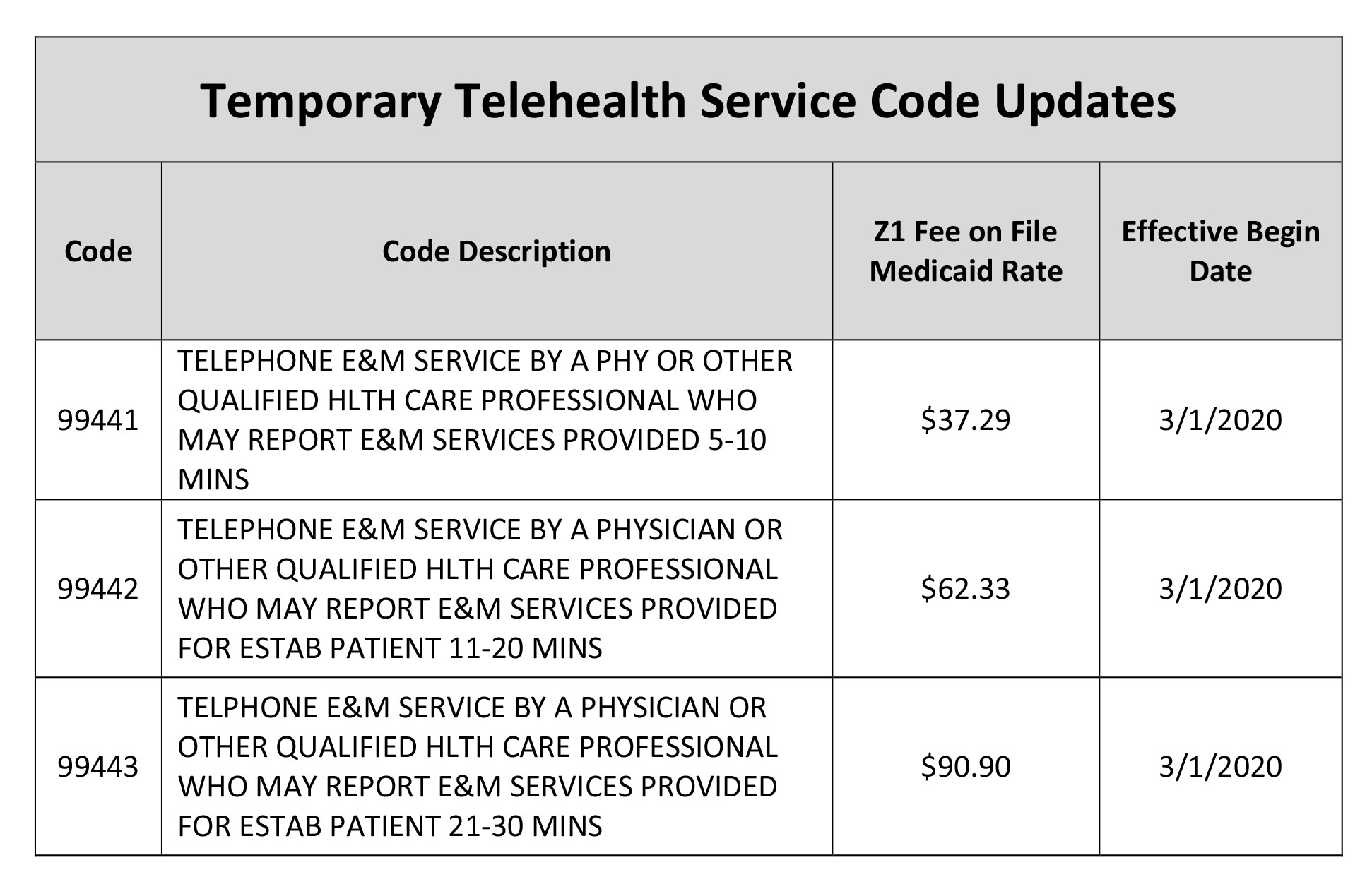
On March 30 CMS issued an Interim Final Rule and released new guidance on how to code and bill for rapidly evolving telehealth services. The Australian Nursing and Midwifery Federation has published Guidelines for telehealth on-line video consultation funded through Medicare.
 Telehealth S Opportunities In New Medicare Advantage Rule
Telehealth S Opportunities In New Medicare Advantage Rule
Further providers must have in-person visits on a regular interval to be determined by the Health and Human Services Department for telehealth.
Telemedicine medicare guidelines. Establish patient identification and document the encounter in the medical record. Broadened access to Medicare telehealth services so beneficiaries can get a wider range of services from their doctors and other clinicians without traveling to a health care facility. MEDICARE TELEHEALTH VISITS.
The new temporary MBS telehealth items are for out-of-hospital patients. There are limited exemptions to this requirement. New Medicare Law Requires In-Person Visit for Telehealth Coverage.
The Australian College of Nurse Practitioners has published resources for nurse practitioners on telehealth. In December 2020 the Consolidated Appropriations Act of 2020 section 123 includes language that requires behavioral health providers to have seen their client in person during the prior six months before a telehealth visit will be covered by Medicare. On March 6 2020 Medicare began temporarily paying clinicians to furnish beneficiary telehealth services residing across the entire country.
You can get certain physical and occupational therapy services at home. It is a legislative requirement that GPs and Other Medical Practitioners OMPs working in general practice can only perform a telehealth or telephone service where they have an established clinical relationship with the patient. Just when you thought you got your head semi-wrapped around Medicare telemedicine rules they go and throw it out the window.
Originating Site Expansion. If you have Original Medicare review your Medicare Summary Notice for errors. The provider must use an interactive audio and video telecommunications system that permits real-time communication between the distant site and the patient at home.
First verbal requests to consider medical aid in dying can effectively and legitimately be taken by telemedicine if they. Medicare made these changes to telehealth in 2020. Perform a concise history of present symptoms and treatments from the patient including palliative care modalities in effect.
You can get Medicare telehealth services for certain emergency department visits at home. Before you file another claim here are the three sweeping changes you must. The median intraservice time is the time spent face-to-face with the provider and the total time includes services such as reviewing tests prior to the visit.
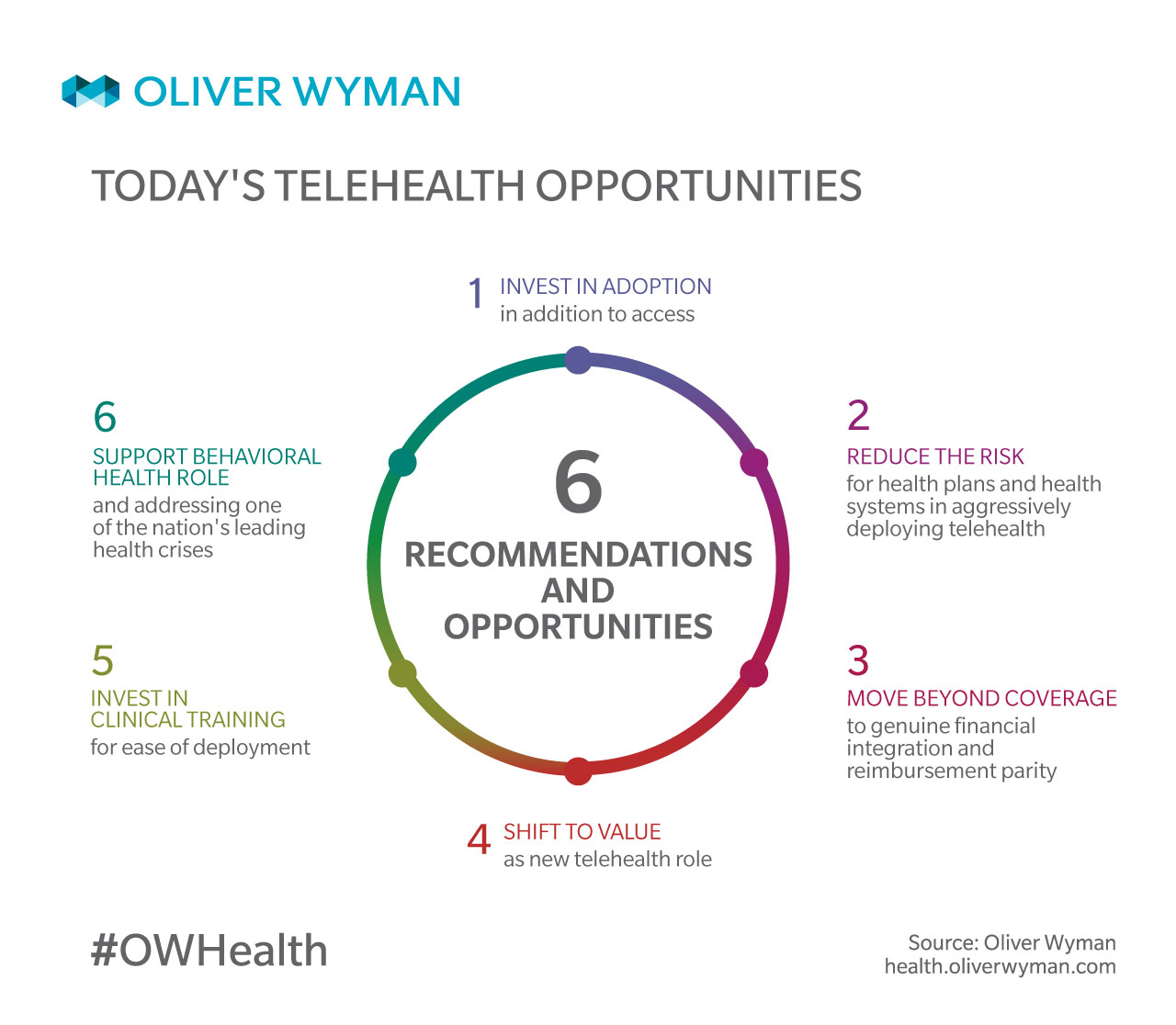
Provide telehealth recommendations for consideration and endorsement by Taskforce for provision to Government. In response to the pandemic and need to quickly scale and expand the reach of telemedicine Governors regulators and legislators in many. Currently Medicare patients may use telecommunication technology for office hospital visits and other services that generally occur in-person.
Beginning on March 6 2020 Medicare administered by the Centers for Medicare Medicaid Services CMS will temporarily pay clinicians to provide telehealth services for beneficiaries. The Medicare Benefits Schedule MBS Review Taskforce the Taskforce is reviewing how more than 5700 Items on the MBS can be aligned with contemporary clinical evidence and practice. CMS telemedicine guidelines state that providers may use the typical times assigned in the Calendar Year CY 2020 Medicare Physician Fee Schedule MPFS Final Rule public use file CMS 2020.
If you have other coverage like a Medicare Advantage Plan review your Explanation of Benefits Report anything suspicious to your insurer. Any originating site requirements that apply under Original Medicare are temporarily waived as described below so that telehealth services provided through live interactive audio-video can be billed for members at home or CMS originating site. UnitedHealthcare will extend the expansion of telehealth access for in-network and out-of.
Medicare officials have stated that services provided via audiovisual equipmentsuch as a smartphone or platforms like FaceTime or Skype in the same building as the patient or through the patients window are allowed but are considered in-person services and. Telemedicine policy recommendations best practices Prior to the COVID-19 pandemic many states had laws in place that allowed broad coverage of telemedicine services and payment parity with in-person services. Report anything suspicious to Medicare by calling 1-800-MEDICARE 1-800-633-4227.
You can get Medicare telehealth services at renal dialysis facilities and at home. Medicare covers some services delivered via audio only devices.